The original organics
About 10,000 years ago there were literally no farmers, and for tens of thousands of years humans had become quite widespread around different pockets of Asia, Oceania, Africa and the North & South America. The Earth’s hunting and gathering population were sufficiently small enough at the time to allow people to exist comfortably on the land, there was certainly plenty of it and little competition with such a small global population. One can only imagine the quality of produce in terms of the mineral and vitamin content and completely free of chemicals, a far cry from today’s farming methods which rely heavily on chemicals to kill pests and fertilise a depleting soil. Foods were not processed; there were no factories and certainly no supermarkets. Crops today are grown as fast as possible, picked often before they are naturally ripe or fully mature and often transported for many miles and stored sometimes for long periods of time before they reach the consumer.

A changing diet in a changing world
A number of converging forces coincided with a changing climate to make mechanised agriculture a necessity. Steady population growth over many thousands of years has ensured increasing competition for land. Global warming has certainly changed the way we view our environment today, but even after the last Ice Age, the world started to warm up more making the Earth’s climate warmer and a bit wetter.
This change was a real bonus to all the wild grasses growing at the time, including the ancient ancestors of today’s cereal grains, which became widespread and abundant and even more attractive as a viable food source. As the wild grasses were increasingly used for food, they were modified and slowly bred into types more appropriate for farmers.
Certain strains were bred to suit local climatic conditions, soil and water types. Wheat, in particular, has been selectively bred for many thousands of years to ensure for example the seeds didn’t detach easily from the stem or fall victim to pests and diseases as was the case of wild varieties. According to Dr Boyd Eaton, author of “The Paleolithic Prescription”, agriculture was present about 5,000 years ago on all inhabited continents except Australia. This book made me understand how and why humans so radically modified foods such as wheat over the years.
The impact of a changing diet
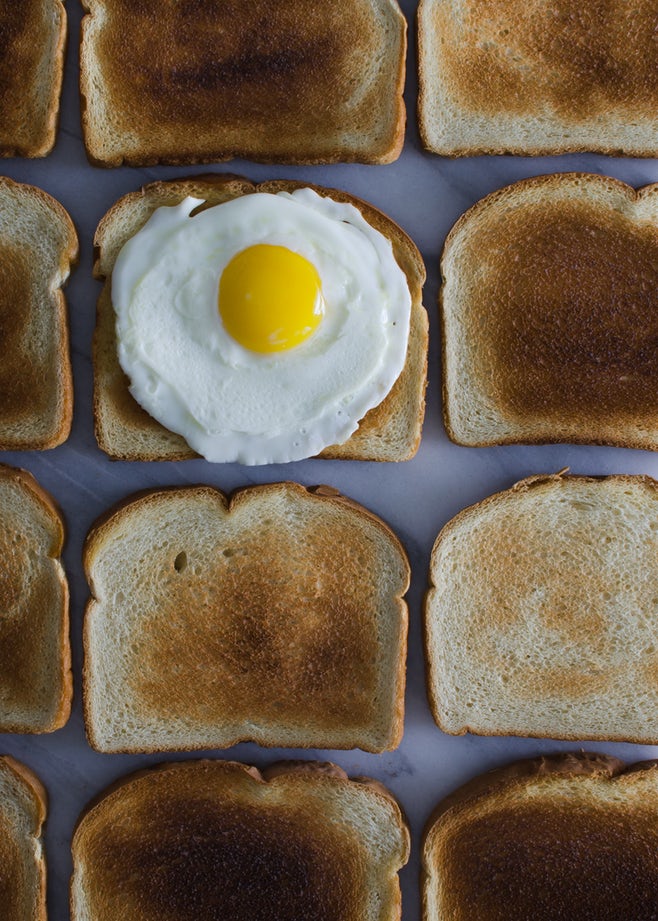
There is fairly strong evidence that 10,000 years ago most humans did not consume many grains at all and, certainly no toast with jam and a cuppa each morning. Humans were hunter-gatherers who subsisted mostly on vegetables and meats. But, 10,000 years is a very short time in a biological sense for humans: in fact, over 99 percent of our genetic make-up was already in place before we ever started consuming wheat and making our daily bread. Our digestive systems have not really changed much at all biologically over tens of thousands of years – but our diets, especially the grains we consume, are a far cry from what they used to be.
 How can our bodies possibly cope with the fact that our grains have become so incredibly modified in such a short time? They can’t, and very little attention is paid to this fact when a person suffers from an ongoing chronic health complaint, at times for many years, where no cause can be found. Remember Hippocrates, the father of medicine, who once said – “Let food be your medicine, and medicine be your food”. How can we truly call commercial supermarket bread today a food, let alone a “medicine”?
How can our bodies possibly cope with the fact that our grains have become so incredibly modified in such a short time? They can’t, and very little attention is paid to this fact when a person suffers from an ongoing chronic health complaint, at times for many years, where no cause can be found. Remember Hippocrates, the father of medicine, who once said – “Let food be your medicine, and medicine be your food”. How can we truly call commercial supermarket bread today a food, let alone a “medicine”?
When considered from this dietary genetic perspective alone, it is not too surprising that the sheer amount of refined carbohydrates and grains many now consume can cause a wide array of health issues. Contemporary humans have not suddenly evolved mechanisms to incorporate the high carbohydrates including starch and sugar-rich foods into their diet. Remember, for tens of thousands of years humans lived on meat and vegetables, and never on white bread, breakfast cereals, crackers, biscuits, two-minute noodles, two-minute microwave porridge, and tinned spaghetti.
Gluten
Take for example gluten, a valuable complete plant protein found mainly in wheat, oats, barley and rye. Gluten’s main protein is called gliadin, a water-insoluble protein giving extensibility to cereal grain flours, and it is the gliadin that causes the problems with our immune systems.
Globally, much more wheat flour is produced than any other flour.
- “Hard” flour like bread flour is high to very high in gluten, with a certain toughness that holds its shape well once baked.
- “Soft” flour is comparatively low in gluten and so results in a finer texture. Soft flour is usually divided into cake flour, which is the lowest in gluten, and pastry flour, which has slightly more gluten than cake flour.
Gluten, dried and milled to a powder and added to ordinary flour dough, improve rising and increases the bread’s structural stability and chewiness. Kneading promotes the formation of gluten strands and cross-links, so a baked product is chewier in proportion to how much the dough is worked.
 Gluten is also used as a stabilising agent in products like ice-cream and tomato ketchup, where it may be totally unexpected. Foods of this kind present a problem because the hidden gluten constitutes a hazard for people with true celiac disease.
Gluten is also used as a stabilising agent in products like ice-cream and tomato ketchup, where it may be totally unexpected. Foods of this kind present a problem because the hidden gluten constitutes a hazard for people with true celiac disease.
In the United States, gluten may not even be listed on the labels of such foods because the U.S, Food and Drug Administration has classified gluten as GRAS (Generally recognised as safe. In the United Kingdom, only cereals currently need to be labelled, while other products are voluntary. In fact, in the UK most gluten-free food is clearly labelled so, as is non-gluten-free food, in NZ.
What is Celiac Disease (CD)
When people with CD eat gluten, an immune reaction occurs that causes the villi, (hair-like projections in the small intestine that absorb nutrients), to become damaged, which interferes with the body’s ability to absorb nutrients such as proteins, carbohydrates, fats, vitamins, minerals, even water in some cases. Over time this inability to absorb nutrients and damage to the small intestine can result in serious side effects.
One of the major problems with CD is that it can go undetected for many years because symptoms are not always present. And because CD has been considered a “rare” disease up until now, it often goes undiagnosed or is misdiagnosed as “irritable bowel syndrome” or “lactose intolerance”. Although the cause of the disease is not known, it appears that certain triggers such as severe emotional stress, surgery, viral infection or even pregnancy can activate CD in some people. This is often because the powerful immune-boosting and anti-inflammatory hormone cortisol, produced by your adrenal gland, can diminish over time due to continual low-grade stress. Immunity drops under the presence of low cortisol, and allergies may well be the result, particularly towards the more commonly allergy prone proteins such as beta-casein (milk) and gliadin (wheat).
Wild wheat grain contains only about 3-5% gluten content. Modern hybridisation, hormonal treatment and artificial fertilising have all increased the gluten content of modern grains such as wheat by up to an amazing 30%. Many bakers now even add extra gluten to the dough to extend shelf-life.
A study in the Journal of Paediatrics (January 2000) screened 1,200 children aged 6 months up to 20 years with blood tests and, in some cases, small intestinal biopsy. The researchers reported that the prevalence of celiac disease (CD) in these patients ranged from 1 in 33 to 1 in 57. Previous studies have shown that about 1 in 250 people in Europe had celiac’s disease, and 1 in 5,000 in America. According to another more recent study In the United States, it took as many as 12 to 13 years after symptoms occurred for patients to be diagnosed with celiac disease until only quite recently.
We now know that CD, and different variants or types of CD are much more common than originally thought. I am not that convinced with the reliability of wheat or gluten testing, in my clinical experience I have seen too many patients over the years improve considerably once we removed wheat products from their diet (essentially their favourite wheat based foods), regardless of what the test results said.

Gluten intolerance or a wheat allergy?
The Journal of Paediatrics study is quite important, as it highlights something I have known all along – that Western medicine typically has very little understanding of how human health can be so adversely and commonly affected by something as basic as the very bread most of us consume. We have the same problem with cow’s milk; years ago I once tested over 300 children in a two year period who suffer from eczema, hayfever, recurring acute ear nose and throat problems and asthma. I found that cow’s milk allergies were common in 68% of these immune-compromised cases.
I have almost always found a positive correlation with dairy testing over wheat testing. Meaning, if dairy is “positive” in an allergy test; the person will improve quite a lot when we remove the offending food. In my experience, I have found it easier to get “false negatives” with wheat testing than with dairy testing. It is my belief that there are many other proteins in wheat causing allergic problems, which are not tested for, particularly Omega-5 gliadin.
Wheat allergy may be a misnomer because there are many allergenic components in wheat, and different responses are often attributed to the many different proteins. And, how can we possibly test a person for all these different proteins? If in doubt, leave wheat out for a few weeks.
Diagnoses of wheat allergy deserve special consideration because they are often overlooked in the clinic. Omega-5 gliadin, the most potent wheat allergen, cannot be detected in whole wheat preparations, and it must be extracted and partially digested (similar to how it degrades in the intestine) to reach full activity. A Japanese study in 2004 revealed that digestion of wheat proteins can increase the allergic response by 10 fold, and that almost all types of allergy testing may not be suitable to detect every single type of wheat allergy. Wheat allergies were once a common occurrence, causing contact dermatitis.
 For example, a primary cause was the donning agent (powder) used for latex gloves prior to the 1990s, however, most gloves now use protein-free starch as donning agents. A study of mothers and infants on an allergen-free diet demonstrated that atopic dermatitis, eczema and urticaria can be avoided if wheat sensitive people in the population avoid wheat in the first year of life. This is similar to milk allergies.
For example, a primary cause was the donning agent (powder) used for latex gloves prior to the 1990s, however, most gloves now use protein-free starch as donning agents. A study of mothers and infants on an allergen-free diet demonstrated that atopic dermatitis, eczema and urticaria can be avoided if wheat sensitive people in the population avoid wheat in the first year of life. This is similar to milk allergies.
And yet, very few doctors will routinely tell a parent to stop giving milk or bread products to their child for a trial period to see if the symptoms improve. I do – and the results just speak for themselves, the proof of the (wheat and dairy free) pudding is in the eating.
When to avoid wheat
Wheat, especially commercially baked bread, is not bad for everyone, just most folk with ongoing health problems they can’t seem to get to the bottom of, and I guess that this makes up a lot of the population!
There is no doubt in my mind that if you are overweight you would best to avoid wheat products as much as possible, even organic whole-wheat products, as they will contribute to elevated insulin levels that will disrupt your biochemistry and impair your ability to lose weight.
Carbo-HYDRATES are exactly what the name says, they “hydrate” you and you may end up being a permanent “puffy” member of the BBC. (The Big Bum Club).
Unfortunately, many patients I see are very much addicted to their breads, bagels, croissants, pizza, pasta, waffles and pancakes and many “would rather die” than give up their cheese and crackers in the afternoon or that piece of toast in the morning.
 What about the sub-clinical cases of CD?
What about the sub-clinical cases of CD?
These people are the ones who have issues with wheat, yet appear to be fine with the gluten anti-body blood test and the small intestine biopsy, as well as the conventional medical RAST (scratch test) for wheat allergies. They are the “walking wounded” and suffer silently with function digestive problems.
These patients may have bloating, burping, over or under acidity, constipation, diarrhoea of a host of other digestive or skin problems they put up with, sometimes for many years. They go to the GP, referred to a bowel specialist – every test is done, they are scoped, prodded, scanned, stool tests, blood tests. The diagnosis, if any is ever made, may be conveniently called “irritable bowel syndrome”.
Imagine taking your (slightly) sick car to the mechanic, who after an hour of head scratching says that your car has “irritable motor syndrome”. The mechanic has not found a solution, just labeled your car with a fancy name. You are told to put up with your irate motor.
If your tummy plays up, simple – change your diet first
Stay with the change for some time (6-8 weeks), not 5 minutes please!
Remember, if your car won’t start and you call the mechanic, they will be quick to ask you “did you check the fuel first”. In my clinical experience, many patients I see in the clinic may well unknowingly have a problem with a common grain such as wheat, and are best to avoid wheat in particular from their diets until at least they can establish that gluten or other wheat protein is not the problem.
Most people don’t realise that there are many potential reactions to wheat, aside from celiac disease and gluten that can cause health problems.
It is amazing how many people’s chronic health complaints I have seen clear up once they stop wheat altogether. Some well known and highly experienced and respected American and European clinicians firmly believe that very few can adequately digest the protein in wheat called gliadin. And we have not even motioned the cross-reactions occurring in your digestive system involved when you eat bread/s and then consume coffee, tea, alcohol or other sweet foods or drinks along with the wheat products.
Small Intestine Biopsy is the Only True Diagnosis of CD
In a 1994 study, blood had been examined for the presence of anti-gliadin antibodies, which are specificity to celiac patients, was taken from 3,654 students aged 7 to 16 years. It was found that although 56 of the children tested positive for the CD, only 10 had been diagnosed with actual celiac disease in 2001, seven years after an antibody positive blood test. Researchers then did a biopsy of the intestines of 56 of the children who had tested positive to check against the blood test results in 2001.
Of these children, 27 had signs of celiac disease according to the biopsy. The only real diagnosis is by way of small intestine biopsy. Are you in doubt? Then check it out by requesting a small intestinal biopsy.
Celiac Disease Symptoms are wide-ranging and may include:
 (many of these symptoms may also be due to a wheat allergy)
(many of these symptoms may also be due to a wheat allergy)
- Bloating, flatus and abdominal cramps, gurgling sounds
- Chronic diarrhea or constipation.
- Osteoporosis
- Central and peripheral nervous system disease
- Unexplained anemia
- Weight loss or weight gain
- Tooth enamel defects
- Fatigue, poor appetite
- Infertility
- Depression
- Dermatitis Herpetiformis (DH), a skin condition that causes intense itching and blistering (elbows, knees, buttocks especially)
- Vitamin K deficiency (associated with risk for hemorrhaging)
- Impairments in a child’s mental functioning that could cause or aggravate autism, Asperger’s syndrome, ADD or even schizophrenia. Is your child autistic? Go wheat and dairy free.
Gluten and severe headaches – 78% of subjects reacted to wheat
According to the results of a small study, some people may experience migraine headaches due to wheat. The study showed that these patients had a sensitivity to gluten, and magnetic resonance imaging scans (MRI) suggested they had actually had an inflammation in the central nervous system (brain).
Nine of the ten patients tried a 100% gluten-free diet, and seven stopped having headaches. Two other patients had some – but not complete – success by switching to a gluten-free diet. One patient did not follow the diet.
Migraine sufferers were tested for food allergies to various foods. Do you have bad headaches? Have you tried everything but still like you sandwiches and toast? Try giving up gluten 100% for a few weeks and see what happens.
The moral of this story, is that if you have a chronic health such as a headache, skin or digestive issue, or any one of a host of chronic on-going health issues, try avoiding all wheat products for two weeks and see if you improve.
That approach is certainly far less expensive and more accurate than any diagnostic technique currently available. You may not even require that expensive poke, prod, camera or other investigative procedure after all.
Mr Eric Bakker B.H.Sc.(Comp.Med) ND RC Hom.
Read more from Eric on GrownUps here.
References
- The Paleolithic Prescription S Boyd, MD. Majorie Shostak, Melvin Konner, MD, PhD. Harper Row Publishers 1989.
- New England Journal of Medicine June 19, 2003;348:2517-2524,2568-2570
- Journal of Paediatrics (January 2000 136:86-90)
- Neurology February 2001;56:385-388
- Grant, E. C. Food allergies and migraine. Lancet. 1(8123):966-969, 1979.
- Matsuo H, Morita E, Tatham AS, Morimoto K, Horikawa T, Osuna H, Ikezawa Z, Kaneko S, Kohno K, and Dekio S. (2004).
- “Identification of the IgE-binding epitope in omega-5 gliadin, a major allergen in wheat-dependent exercise-induced anaphylaxis.”. J Biol Chem. 279 (13): 12135–12140.
- Zeiger RS, Heller S, Mellon MH, et al (1989). “Effect of combined maternal and infant food-allergen avoidance on development of atopy in early infancy: a randomized study”. J. Allergy Clin. Immunol. 84 (1): 72–89.





Valerie - 6 years ago
Yes, I agree. Informative and helpful, looking forward to Part 2.
Thank you.