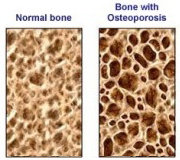
The conventional approach
The current mainstream medical approach of osteoporosis prevention and management is limited to the use of HRT, and the very poorly absorbed calcium carbonate form of calcium (Doctors, what about the other minerals and trace elements?). Other options include medications such as estrogens and anti-absorptive drugs such Alendronate (Fosomax), Etidronate (Etidrate) and Calcitriol (Rocalcitrol). Long term drug safety has not been established, although extensive studies are on-going. While these prescriptions may be clinically useful for some, their safety and efficacy is highly questionable, and they never address each woman’s unique and often complex cause for osteoporosis in the first place. Mum took Fosomax for over ten years, believing it would save her, it did nothing. Her GP would have been better off getting her to understand the real causative factors here, because osteoporosis does not really exist in the undeveloped nations.
Diet and Bone Health
Diet has a significant effect on bone health. In the book, "Paleolithic Nutrition," the author demonstrated that the diet of the hunter-gatherer populations of 40,000 years ago contributed to their quite massive bone density. This diet was about 35% meat and 65% vegetables and fruit. Sorry folks, no flat-whites, fish and chips, cold-beer, or typical Kiwi fare in those days. There was little or no cereal grain consumption and absolutely zero dairy food, and a cow never stood still long enough to be milked before it was eaten! The diet was naturally low in sodium (690 mg) and high in calcium (1580 mg). High dietary intakes of salt and sugar, common in the standard NZ diet, cause increased urinary calcium excretion and should be reduced. I have always wondered why the countries with the highest milk consumption are also the countries with the highest rates of osteoporosis. Forget the cow folks, do you still think that without milk your bones will crumble?
The goal in my clinic is to counsel patients to eat a nutrient-dense diet so that supplementation is kept as minimal as possible. Teaching concepts of a whole foods diet, with particular emphasis on increasing the intake of non-starchy vegetables, fresh fruits, nuts and seeds, introducing people to sea vegetables, and reducing their intake of refined carbohydrates and grains will reduce their need for supplements as well as improve their overall health.
Exercise and Bone Health
Exercise has a central role in the prevention and treatment of osteoporosis. No drug, hormone or mineral such as calcium, can cause a skeleton to be heavier or sturdier than required by the uses to which the owner puts it.
Peak bone mass is achieved both by adequate bone-building nutrients and by mechanically loading the skeleton. In order for exercise to be effective it must be continued throughout life. Simply put, inactivity leads to bone loss. In a study of 200 individuals 70 years of age or older doing Tai Chi, there was a 47.5% reduction of risk of multiple falls! 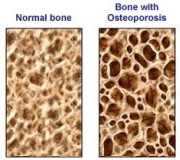
Mum was into Tai Chi and practiced this wonderful “meditation in motion” for over twenty years. But – because she didn’t get involved in the “complete package” of adopting the correct lifestyle and diet, it didn’t have the desired effect. Range of motion in the lower extremities showed significant improvement, and lower blood pressure was observed following Tai Chi participation.
What I like about Tai Chi is that improves the coordination, muscle strength and flexibility, so that a slip does not become a fall and a fall does not become a fracture. Exercise also reduces the older person’s need for many different medications that can alter balance and coordination and result in a fall. The elderly shouldn’t have to be pill poppers as too many are.
Some folk say that the best exercise program of all to maintain bone density however is yoga. It is weight bearing, and in the various yoga postures the muscles pull on the bone, thus stimulating additional bone remodeling.
 Vitamin D
Vitamin D
We all know the dangers of too much sun. But are we aware of the health effects of too little?
People living in NZ may be at increased risk of vitamin D insufficiency and its associated risk of fractures caused by osteoporosis because they are not exposed to enough sunshine – a source of vitamin D. Short exposures to the sun (15 minutes) per day will also do the trick, as will consumption of vitamin D-rich foods such as eggs, chicken livers, fish oil, and fish like salmon, sardines, herring, mackerel, and halibut. Vitamin D is one of the most important hormone nutrients affecting bone, with its role in regulating intestinal and renal absorption of calcium. Vitamin D deficiency has been found in 25% of elderly patients presenting with hip fracture. Several studies suggest a daily supplement of 1000 units a day of vitamin D, at least during the winter. A recent article in the Medical Journal reminds readers that cod liver oil, (very rich source of vitamin-D), has been a reliable remedy for rickets since the 1600s.
Nutrients and Bone Health
Calcium
The benefits of calcium supplementation on osteoporosis have received considerable attention, and unfortunately these supplements are considered to be a cure-all by many. It must always be remembered that calcium is an integral part of any comprehensive approach to osteoporosis, but calcium alone is not the answer to osteoporosis. There are many forms of calcium available for supplementation, but the benefit of supplementation is closely related to its absorbability. When compared with an equal dose of elemental calcium from calcium carbonate, 500 mg elemental calcium from calcium citrate was the most effective at increasing bone density in post-menopausal women. Recent studies have shown that it may be dangerous to give calcium unopposed by magnesium to women who are postmenopausal as it may increase the risk of a heart attack considerably.
Magnesium
Sixteen of nineteen osteoporotic women demonstrated low bone magnesium and abnormal crystalline structure of the bone. Magnesium supplementation (250-750 mg/day) appears to significantly increase bone density and reduce the incidence of fracture. The appropriate intake ratio of calcium to magnesium is controversial, with some authors supporting the current 2:1 ratio and others recommending a 1:1 ratio.
Vitamin K
Vitamin K is important to the maintenance of healthy bone. Because 90% of the vitamin K in the human liver is made by the intestinal flora, impaired vitamin K status should always be considered in anyone with frequent or long-term antibiotic treatment. Vitamin K is fat soluble and can be mal-absorbed in those with chronic digestive problems or with malabsorption. Vitamin K is found in green leafy vegetables, and legumes.
 Boron
Boron
Many human studies suggest that boron interacts with other nutrients and plays an important regulatory role in bone metabolism. In post-menopausal women, boron supplementation at 3 mg per day significantly reduced the urinary excretion of calcium and magnesium.
Trace Minerals
Several trace minerals, especially copper, zinc, and manganese, are essential in bone metabolism as co-factors of specific enzymes in bone development and mineralisation. In a study of 59 post-menopausal women, the effects of calcium supplementation (as calcium citrate, 1000 mg elemental Ca/day) with and without the addition of zinc (15.0 mg/day), manganese (5.0 mg/day) and copper (2.5 mg/day) on the lumbar spine was evaluated over two years. Bone loss was arrested the most in the-calcium-plus-trace-minerals group.
Hormones
Estrogen inhibits bone breaking down activity as well as stimulating calcium absorption by the intestine, and facilitates the synthesis of vitamin D. It is well documented that estrogen replacement therapy decreases bone resorption and helps to stabilise bone mass, but confers only a 2% increase in bone density at best, and must be taken for ten or more years to reduce fracture incidence. Unfortunately, this approach subjects women to a long-term therapy that poses an unacceptable increasing risk of breast cancer, blood clots, strokes, uterine cancer and many other side effects.
Progesterone, the much safer option, is also active in bone metabolism and appears to promote bone formation. Some researchers state that post-menopausal osteoporosis may in fact be in part a disease of progesterone deficiency. In a study of 100 post-menopausal women followed for three years, Dr. John Lee reported the significant benefit of progesterone which was independent of supplemental estrogen. The treatment of osteoporosis with progesterone appears quite encouraging and deserves significantly more research.
Lifestyle and Bone Health
 Alcohol & coffee consumption and cigarette smoking are associated with osteoporosis. Alcohol inhibits absorption and increases excretion of calcium, magnesium, ascorbic acid, zinc and copper. Caffeine in average daily doses of two to three cups accelerates bone loss from the spine and total body in women with calcium intakes below 800 mg/day. Cigarette smoking depletes the body of vitamin C and exposes it to a number of toxins, such as cadmium and lead, which directly damage bone and interfere with calcium absorption.
Alcohol & coffee consumption and cigarette smoking are associated with osteoporosis. Alcohol inhibits absorption and increases excretion of calcium, magnesium, ascorbic acid, zinc and copper. Caffeine in average daily doses of two to three cups accelerates bone loss from the spine and total body in women with calcium intakes below 800 mg/day. Cigarette smoking depletes the body of vitamin C and exposes it to a number of toxins, such as cadmium and lead, which directly damage bone and interfere with calcium absorption.
Modification of these habits is essential to any bone-building program. Do you smoke and drink alcohol regularly and have three or more cups of coffee a day and expect great bone density as you age? Self delusion is the worst form of delusion I’ve been told.
Conclusion
I’d like you to always remember this, that the health of your skeleton is a reflection of the total health of your body. Osteoporosis can be prevented, but one must start early! Osteoporosis prevention and treatment is an opportunity not only to address skeletal concerns, but also to make a positive impact on your total health and well-being. So typical, like many chronic complex illnesses, the current medical idea of osteoporosis prevention and treatment fails to address both main causes and the chronic systemic dysfunctions that lead to osteoporosis in the first place.
Do you have an elderly relation who is frail, who has low bone density and has broken bones in the past very easily? I’d like you to make sure that you aware that she is like a “candle in the wind” and can easily succumb to a broken hip all too easily. Make every day count with your loved one.
The only really practical and common sense approach to osteoporosis is a preventative and restorative program that includes educating a person in the correct diet, exercise and lifestyle factors which enhance and maintain bone density, and include additional nutrients when needed as required.
An approach like this will improve overall health, reducing needless hospitalisation whilst sparing a person from misery and a potentially-hazardous drug-induced therapy. It wasn’t nice seeing my own mother suffer with osteoporosis in her later years, and if this article can help just one younger person to grasp the full significance of the prevention of osteoporosis it will have been worth the time and effort I put into researching and writing it.
References
1. Dempster DW, Lindsay R. Pathogenesis of osteoporosis. Lancet 1993;341:797-801.
2. Heaney, R. The Osteoporotic Syndrome. New York, NY: Wiley – Liss, Inc.;1993:139-144.
3. Wolf, SL, Barnhart HX, Kutner NG, et al. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Journal American Geriatric Society 1996;44:489-497.
4. Krane SM, Holick MF. Metabolic Bone Disease: Osteoporosis. In: Isselbacher K, Brunwald E, Wilson, J, et al., eds. Harrison's Textbook of Internal Medicine. New York, NY: McGraw Hill, Inc.;1994:2172-2176.
5. Lindsay R. Managing osteoporosis: Current trends, future possibilities. Geriatrics 1987;42:35-39.
6. Weiss RF. Herbal Medicine. Gothenberg, Sweden: AB Arcanum; 1988:318.
7. Lee J. Osteoporosis reversal: The role of progesterone. International Clinical Nutritional Review 1990;10:384-391.
8. Dawson-Hughes B, Dallal GE, Krall EA, et al. A controlled trial of the effect of calcium supplementation on bone density in post-menopausal women. New England Journal of Medicine 1990;323:878-883.
9. Cohen L, Kitzes R. Infrared spectroscopy and magnesium content of bone mineral in osteoporotic women. Israel Journal of Medical Science 1981;17:1123-1125.
10. Sojka JE, Weaver CM. Magnesium supplementations and osteoporosis. Nutritional Review 1995;53:71-74.
11. Abraham GE, Grewal H. A total dietary program emphasizing magnesium instead of calcium. Journal of Reproductive Medicine 1990;35:503-507.
12. Shearer MJ. Vitamin K. Lancet 1995;345:229-234.
13. Pizzorno J, Murray M. Osteoporosis. Textbook of Natural Medicine. Seattle, WA: Bastyr Books; 1989.
14. Naghii MR, Samman S. The role of boron in nutrition and metabolism. Progressive Foods Nutritional Science 1993;17:331-349.
15. Strause L, Saltman P, Smith KT, et al. Spinal bone loss in post-menopausal women supplemented with calcium and trace minerals. Journal of Nutrition 1994;124:1060-1064.
16. Harris SS, Dawson-Hughes B. Caffeine and bone loss in healthy post-menopausal women. American Journal of Clininical Nutrition 1994;60:573-578.




Join the Discussion
Type out your comment here:
You must be logged in to post a comment.